Name: Gnana Prasuna Reddy K.
Roll no. 49
9th semester
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
13 year old male patient complaining of yellowish discolouration of eyes and yellow urine.
Following is a brief about the case,
(History as per date of admission).
CHIEF COMPLAINTS:
A 13 year old male child, studying in grade 7 at a school in Miryalguda was brought to the Medicine OPD (on 6/01/2022) with complaints of:
• Yellowish discolouration of eyes since 9 days
• Dark coloured urine since 9 days.
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic as a newborn - healthy term baby, cried immediately after vaginal delivery.
He had physiological jaundice that resolved spontaneously.
He is immunized as per schedule.
At 8 months of age: he developed altered bowel habits - 1 week of passage of loose stools followed by 1 week of passing normal stools.
Later he continued to pass loose stools for 2-3 months and became cachetic.
He was taken to the hospital where he was given IV antibiotics and 2 FFP transfusions.
He recovered in about 3 months time and according to hospital discharge summary, he was suspected to be suffering from :
• Celiac disease
• Chronic diarrhea
• Chronic Malabsorption
On further inquiry, the parents said that he used to have recurrent cold, coughs and fever. He also has used inhalers - during winters - for 1 year.
He wasn't admitted to a hospital at any point.
There is no history of Pneumonia.
At 9 years of age : parents noticed a swelling in the neck and took him to an ENT doctor. From there he was referred to an endocrinologist where he was diagnosed with Hypothyroidism.
Medication used - Thyronorm - initially 150 mcg, later increased to 180mcg, everyday, now he is on 200 mcg.
There is history of chronic itching over palms and foot since 9 years of age - Dermatologist prescribed medications for dry skin.
At 12 years of age : he had Chicken pox that resolved in about 10 days time.
Now , at 13 years of age :
• It started with two episodes of bilious, non projectile vomiting, before food intake
• Following that, yellow colored urine and yellowish discolouration of eyes was seen
These complaints occured 9 days before hospital admission.
No fever
No pain abdomen
No loose stools/ clay colored stools
No history of small joint pains
He was treated by a local pediatrician, but because of constant rise in bilirubin levels he was referred here for further treatment.
HISTORY OF PAST ILLNESS:
• There is no history of similar complaints in the past.
• He is on regular medication for Hypothyroidism for past 5 years.
• He is not a known case of DM, HTN, ASTHMA,TB, EPILEPSY.
• No history of surgeries in the past.
FAMILY HISTORY:
He is a 4th order child, born out of grade 3 consanguinous marriage.
He had one elder sister - who expired at 5 years of age.
He has 2 elders brothers.
His sister was the first child.
She was asymoptomatic till 2 years of age ,then she developed shortness of breath and was rushed to hospital,where her condition detiorated and had to be admitted.
She was diagnosed to have splenomegaly and her blood counts were decreasing.
She was given multiple blood transfusions, every 25 days,for one year- but remained anemic.
She also underwent bone marrow biopsy twice .
According to parents she was given steriods for one year before her death.
She never had jaundice or recurrent infections.
Eldest brother is 19 year old and second brother is 16.
Second brother had history of fever and white coloured loose stools at the age of 5 years , for which he was taken to the Nalgonda hospital.
He recovered on medication.
He was also diagnosed with anemia from which he recovered with some medications.
No history of Jaundice in this brother.
GENERAL EXAMINATION:
Consent of the patient taken.
The patient is conscious,coherent and cooperative; well oriented to time,place and person.
He is sitting comfortably on the bed.
He is lean built and moderately nourished.
• Height - 156cm
• Weight - 32kgs
• Pallor- present
• Icterus - present
• Clubbing - absent
• Cyanosis - absent
• Lymphadenopathy - absent
• Edema - absent
Vitals:
Temperature: Afebrile
Pulse rate: 100 beats per minute
Respiratory rate: 18 cycles per minute
Blood pressure: 120/70 mm of mercury
He has scars from his recent Chickenpox infection on limbs and trunk.
ABDOMEN EXAMINATION
INSPECTION:
Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving with respiration.
No dilated veins, hernial orifices , sinuses
No visible pulsations
PALPATION:
Soft, non tender
Spleen:
palpable in the left hypochondrium enlarging towards the Right Iliac Fossa , it moves with respiration
It is firm in consistency with a smooth surface and a rounded edge
Liver and Kidney are not palpable.
PERCUSSION:
There is no fluid thrill , no shifting dullness.
Enlarged spleen is dull on percussion.
AUSCULTATION:
Bowel sounds are heard.
CARDIOVASCULAR SYSTEM
INSPECTION:
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse was appreciated
PALPATION:
Apical impulse is felt on the left 4th intercoastal space 2cm away from the midline.
No parasternal heave, thrills felt.
PERCUSSION:
Right and left heart borders percussed.
AUSCULTATION:
S1 and S2 heard , no added thrills and murmurs heard.
RESPIRATORY SYSTEM
INSPECTION:
Chest is bilaterally symmetrical
Trachea – midline in position.
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
Trachea – midline in position.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper/mid/lower interscapular were all RESONANT.
AUSCULTATION:
Normal vesicular breath sounds heard
No adventitious sounds heard.
CENTRAL NERVOUS SYSTEM EXAMINATION.
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
Right. Left
BULK
Upper limbs. N. N
Lower limbs N. N
TONE
Upper limbs. N. N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present , normal
Gait is normal
No involuntary movements
Sensory system - all sensations ( pain, touch, temperature, position, vibration sense) are well appreciated .
INVESTIGATIONS:
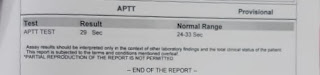
Investigations ordered are : ECG, Hemogram, Bleeding and clotting time, prothrombin time, APTT, Urine analysis, Liver function tests, Renal function tests, Thyroid profile, Blood grouping, cross matching, Direct coombs test, Stool for occult blood and parasites, Serology, USG - Abdomen.
Hemogram:
• There is significant drop in hemoglobin- from 8.9 to recent Hb -5 units.
• Leucopenia.
Urine analysis:
• Salts and bile pigments- positive
Hemoglobin electrophoresis:
Blood grouping and RH typing:
Bleeding and Clotting time:
APTT :
Liver function tests:
Raised bilirubin - both direct and indirect.
Fall in total protein count
Renal function tests:
Sr.CR- 0.7
urea-17
Na+- 141
k+-4
cl- 97
Thyroid profile:
T3-61
T4- 8.66
TSH- 91.85
ANTI TPO ANTIBODIES- 771.1
Direct Coomb’s test- POSITIVE
Stool for occult blood- Negative
Serology:
Negative for HIV, HCV, HbsAg, Dengue, Malaria, Typhoid.
USG abdomen:
Splenomegaly seen.

ECG:
• Spectrum of Autoimmune diseases.
• Autoimmune Hemolytic Anemia.
• Chronic itching of both hands and limbs - suggests CVID (common variable immunodeficiency).
TREATMENT:
• Tab. Thyronorm - 200mcg PO OD.
• Tab. Methylprednisolone - 32mg PO OD.
• Tab. Atarax - 10mg PO OD.
• Physiogel lotion - local application BD
Patient is discharged


















Comments
Post a Comment